Our Health Library information does not replace the advice of a doctor. Please be advised that this information is made available to assist our patients to learn more about their health. Our providers may not see and/or treat all topics found herein.
Ear Infections
Condition Basics
What is an ear infection (otitis media)?
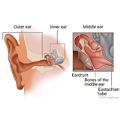
An ear infection is an infection of the middle ear, the area behind the eardrum. This infection is called otitis media. The area can get infected when germs from the nose and throat are trapped there. Ear infections happen mostly to young children. They're the most common kind of ear infection in children.
What causes them?
Middle ear infections are caused by bacteria and viruses. A small tube (eustachian tube) connects your ear to your throat. A cold can cause this tube to swell, blocking it and trapping fluid inside your ear. This makes it a perfect place for germs to grow and cause an infection.
What are the symptoms?
The main symptom is an earache. It can be mild or may hurt a lot. Babies and young children may be fussy. They may pull at their ears and cry. They may have trouble sleeping. They may also have a fever.
How are they diagnosed?
Your doctor will ask about symptoms. Then your doctor will look into your ears. A special tool with a light lets the doctor see if the eardrum is infected and if there is fluid behind it. This exam is rarely uncomfortable. There may be tests, such as hearing tests.
How are ear infections treated?
Most ear infections go away on their own. You can treat them at home with an over-the-counter pain reliever like acetaminophen (such as Tylenol), a warm washcloth on the ear, and rest. Your doctor may give you eardrops that can help with pain.
Do not give aspirin to anyone younger than 20.
Your doctor may prescribe antibiotics. Antibiotics are recommended for children under 6 months old and for children at high risk for complications. But ear infections often get better without them. Talk with your doctor. Whether you use antibiotics will depend on how bad the infection is. For children, it also will depend on the child's age.
Follow up with your doctor if your symptoms don't get better. Sometimes children need to follow up if they are younger than 6 months old or if their infection is severe.
Minor surgery to put tubes in the ears may help for repeat infections or hearing problems.
How can you prevent them in children?
There are many ways to help prevent ear infections. For example, don't smoke around children. Encourage them to wash their hands. Make sure your child doesn't go to sleep while sucking on a bottle. And have your child immunized.
Cause
Middle ear infections are caused by bacteria and viruses. Bacteria cause many ear infections.
Swelling from an allergy or an infection in the nose, sinuses, or throat can block the eustachian tubes, which connect the middle ears to the throat. Because of the blocked tube, air can't reach the middle ear. This creates a vacuum and suction, which pulls fluid and germs from the nose and throat into the middle ear. The swollen tube prevents this fluid from draining. The fluid is a perfect place for bacteria or viruses to grow into an ear infection.
Inflammation and fluid buildup can occur without infection and cause a feeling of stuffiness in the ears. This is known as otitis media with effusion.
What Increases Your Risk
Some things that increase your child's risk of a middle ear infection are out of your control. These include:
- Being 3 years old or younger.
- Birth defects or other medical conditions, such as cleft palate or Down syndrome.
- A weakened immune system.
- A family history of ear infections.
- Allergies that cause long-term stuffiness in the nose and can block one or both eustachian tubes.
- Repeated colds and upper respiratory infections.
Other things can increase your child's risk of ear infection. They include:
- Being exposed to cigarette smoke.
- Lying flat while bottle feeding.
- Using a pacifier.
- Using a bottle instead of breastfeeding.
Things that increase the risk of repeated ear infections include:
- Being in a childcare center with many other children.
- Getting the first ear infection before 6 months of age.
- Having persistent fluid behind the eardrum.
- Having an ear infection in the last 3 months, especially if it was treated with antibiotics.
Prevention
These are some things that may help prevent ear infections.
- Don't smoke.
Ear infections are more common in children who are around cigarette smoke in the home. Even fumes from tobacco smoke on your hair and clothes can affect the child.
- Breastfeed your baby.
There is some evidence that breastfeeding helps reduce the risk of ear infections, especially if they run in your family. If you bottle-feed, don't let your baby drink a bottle while your baby is lying down.
- Wash your hands often.
Hand-washing stops infection from spreading by killing germs.
- Make sure your child receives all the recommended immunizations.
- Take your child to a smaller child care center.
Fewer children means less contact with bacteria and viruses. Try to limit the use of any group child care, where germs can easily spread.
- Do not give your baby a pacifier.
Try to wean your child from their pacifier before about 6 months of age. Babies who use pacifiers after 12 months of age are more likely to get ear infections.
Learn more
Symptoms
The main symptom is an earache. It can be mild, or it can hurt a lot. A fever may be present. Babies and young children may be fussy. They may pull at their ears and cry. They may have trouble sleeping.
Symptoms of a middle ear infection often start a few days after the start of a cold or other upper respiratory infection. Some people don't have any symptoms.
If the eardrum ruptures, you may see thick, yellow fluid coming from the ears. This usually makes the pain go away. The eardrum usually heals on its own.
When fluid builds up but doesn't get infected, the ears may just feel plugged. This can affect hearing, but hearing usually goes back to normal after the fluid is gone. It may take weeks for the fluid to drain away.
What Happens
Middle ear infections usually occur along with an upper respiratory infection, like a cold. Fluid builds up in the middle ear. Bacteria or viruses can grow in this buildup into an ear infection.
The fluid pushes against the eardrum, causing pain. It may cause problems hearing. Fever typically lasts a few days. Pain may last for a few days, but young children may have pain for more than a week.
In severe cases, too much fluid can increase pressure on the eardrum until it ruptures and the fluid drains. When this happens, fever and pain usually go away, the infection clears, and the eardrum heals.
Often people still have some fluid behind the eardrum a few weeks after the infection is gone. The fluid may take weeks to months to clear.
Complications, such as an ear infection with chronic drainage, can occur with repeat ear infections.
Complications
Complications from ear infections are rare. But some problems that can occur include:
- Trouble hearing. Hearing problems are usually temporary and mild to moderate. Long-lasting hearing loss is rare. But some children may have problems learning to talk and understand speech if they have repeat ear infections.
- Rupture of the eardrum. If fluid continues to build up in the middle ear, the eardrum may burst. This leaves a small hole that often heals within 2 weeks.
Another complication is ongoing inflammation of the middle ear. The major symptom is repeat or ongoing drainage of pus from the ear through a small hole in the eardrum. Many children with this problem have some hearing loss.
Other complications may develop if there are repeat ear infections:
- Tissue growth behind the eardrum.
- Damage to the tiny bones in the middle ear.
Rare complications include mastoiditis and meningitis.
When to Call a Doctor
Call your doctor now if:
- Your child has sudden hearing loss, severe pain, or dizziness.
- Your child seems to be very sick with symptoms such as a high fever and stiff neck.
- You notice redness, swelling, or pain behind or around your child's ear, especially if your child doesn't move the muscles on that side of the face.
Call your doctor if:
- You've used home treatment for several hours and can't quiet your child who has a severe earache.
- Your baby pulls or rubs their ear and appears to be in pain (crying, screaming).
- Your child's ear pain gets worse even with treatment.
- Your child has a fever with other signs of ear infection.
- You suspect that your child's eardrum has burst, or fluid that looks like pus or blood is draining from the ear.
- Your child has an object stuck in their ear.
- Your child with an ear infection continues to have symptoms (fever and pain) after 48 hours of treatment with an antibiotic.
- Your child with an ear tube develops an earache or has drainage from the ear.
Watchful waiting
Watchful waiting is a wait-and-see approach. Your doctor may recommend it if your child is age 6 months or older, has mild ear pain, and is otherwise healthy. Most ear infections get better without antibiotics. But if your child's pain doesn't get better with nonprescription children's pain reliever (such as acetaminophen) or the symptoms continue after 48 hours, call a doctor.
Exams and Tests
A doctor will diagnose a middle ear infection by doing a physical exam and an ear exam and by asking questions about past health.
The doctor uses a tool called a pneumatic otoscope to look at the eardrum for signs of an ear infection or fluid buildup. For example, the doctor can see if the eardrum moves freely when the otoscope pushes air into the ear.
Other tests may include:
- Hearing tests. These tests are recommended for children who have had fluid in one or both ears for 3 months or if hearing loss is suspected.
- Tympanometry. It measures how the eardrum responds to a change of air pressure inside the ear.
- Tympanocentesis. This test can remove fluid if it has stayed behind the eardrum (chronic otitis media with effusion) or if infection continues even with antibiotics.
- Blood tests. These are done if there are signs of immune problems and a severe infection.
Learn more
Treatment Overview
Most ear infections go away on their own. But antibiotics are recommended for children under the age of 6 months and for children at high risk for complications.
You can treat your child at home with an over-the-counter pain reliever like acetaminophen (such as Tylenol), a warm washcloth on the ear, and rest. Your doctor may give you eardrops that can help your child's pain.
Do not give aspirin to anyone younger than 20.
Your doctor can give your child antibiotics, but ear infections often get better without them. Talk about this with your doctor. Whether you use antibiotics will depend on how old your child is and how bad the infection is.
If your child has cochlear implants, your doctor will probably prescribe antibiotics. That's because serious complications of ear infections, including bacterial meningitis, are more common in children who have cochlear implants than in children who don't have these implants.
Follow-up exams with a doctor are important if your child isn't getting better. The doctor will check for persistent infection, fluid behind the eardrum (otitis media with effusion), or repeat infections.
Fluid buildup and surgery
Doctors may consider surgery for children who have repeat ear infections or who keep getting fluid behind the eardrum. Procedures include inserting ear tubes or removing adenoids and, in rare cases, the tonsils.
Fluid behind the eardrum after an ear infection is normal. And, in most children, the fluid clears up within 3 months without treatment. If your child has fluid buildup without infection, you may try watchful waiting.
Have your child's hearing tested if the fluid lasts longer than 3 months. If hearing is normal, you may choose to keep watching your child without treatment.
If a child has fluid behind the eardrum for more than 3 months and has significant hearing problems, then treatment is needed. Sometimes short-term hearing loss occurs. This is especially a concern in children ages 2 and younger. Normal hearing is very important when young children are learning to talk.
If your child is younger than 2, your doctor may not wait 3 months to start treatment. Hearing problems at this age could affect how well your child can speak. This is also why children in this age group are closely watched when they have ear infections.
Repeat ear infections
If a child has repeat ear infections (three or more ear infections in a 6-month period or four in 1 year), you may want to think about treatment to prevent future infections.
Ear tube surgery may be an option if your child has repeat ear infections. Ear tubes are plastic and are shaped like a hollow spool. They help to clear fluid from your child's middle ear. Allowing the fluid to drain prevents the growth of bacteria that cause ear infections. Your doctor can help you decide if ear tubes are the right choice for your child.
Learn more
Self-Care
Caring for your baby
- Give your child acetaminophen (Tylenol) or ibuprofen (Advil, Motrin) for fever, pain, or fussiness. Do not use ibuprofen if your child is less than 6 months old unless the doctor gave you instructions to use it. Be safe with medicines. Read and follow all instructions on the label.
- If the doctor prescribed antibiotics for your child, give them as directed. Do not stop using them just because your child feels better. Your child needs to take the full course of antibiotics.
- Place a warm washcloth on your child's ear for pain.
- Try to keep your child resting quietly. Resting will help the body fight the infection.
Caring for your child
- Give your child acetaminophen (Tylenol) or ibuprofen (Advil, Motrin) for fever, pain, or fussiness. Do not use ibuprofen if your child is less than 6 months old unless the doctor gave you instructions to use it. Be safe with medicines. Read and follow all instructions on the label. Do not give aspirin to anyone younger than 20. It has been linked to Reye syndrome, a serious illness.
- If the doctor prescribed antibiotics for your child, give them as directed. Do not stop using them just because your child feels better. Your child needs to take the full course of antibiotics.
- Place a warm washcloth on your child's ear for pain.
- Encourage rest. Resting will help the body fight the infection. Arrange for quiet play activities.
Caring for yourself
- Take pain medicines exactly as directed.
- If the doctor gave you a prescription medicine for pain, take it as prescribed.
- If you are not taking a prescription pain medicine, take an over-the-counter medicine, such as acetaminophen (Tylenol), ibuprofen (Advil, Motrin), or naproxen (Aleve). Read and follow all instructions on the label.
- Do not take two or more pain medicines at the same time unless the doctor told you to. Many pain medicines have acetaminophen, which is Tylenol. Too much acetaminophen (Tylenol) can be harmful.
- Plan to take a full dose of pain reliever before bedtime. Getting enough sleep will help you get better.
- Try a warm, moist washcloth on the ear. It may help relieve pain.
- If your doctor prescribed antibiotics, take them as directed. Do not stop taking them just because you feel better. You need to take the full course of antibiotics.
Learn more
Medicines
Antibiotics can treat ear infections caused by bacteria. But most children with ear infections get better without them.
Your doctor will likely give antibiotics if:
- Your child has an ear infection and seems very ill.
- Your child is younger than 2 and has an infection in both ears or has more than mild pain or fever.
- Your child is at risk for complications from the infection, such as trouble hearing.
Other medicines
Other medicines that can treat symptoms of an ear infection include:
- Acetaminophen (Tylenol) or ibuprofen (Advil, Motrin) for pain. Do not use ibuprofen if your child is less than 6 months old unless the doctor gave you instructions to use it. Be safe with medicines. Read and follow all instructions on the label.
- Some eardrops. They may help with severe earache. But don't use them if the eardrum is ruptured.
Most studies find that decongestants, antihistamines, and other nonprescription cold remedies usually don't help prevent or treat ear infections or fluid behind the eardrum.
Do not give aspirin to anyone younger than 20.
Why to avoid antibiotics when they're not needed
Antibiotics often are not needed to treat an ear infection.
- Most ear infections will clear up on their own. This is true whether they are caused by bacteria or a virus.
- Antibiotics kill only bacteria. They won't help with an infection caused by a virus.
- Antibiotics won't help much with pain.
There are good reasons not to give antibiotics if they are not needed.
- Overuse of antibiotics can be harmful. If antibiotics are taken when they aren't needed, they may not work later when they're really needed. This is because bacteria can become resistant to antibiotics.
- Antibiotics can cause side effects, such as stomach cramps, nausea, rash, and diarrhea. They can also lead to vaginal yeast infections.
Learn more
Surgery
Doctors may consider surgery for children who have repeat ear infections or for those who keep getting fluid behind the eardrum. Procedures include inserting ear tubes, removing the adenoids, and, in rare cases, removing the tonsils.
Ear tube surgery
Ear tubes are plastic and are shaped like a hollow spool. They help clear fluid from your child's middle ear. Doctors may suggest tubes for children who have repeat ear infections or when fluid stays behind the eardrum.
During the surgery, the doctor makes a hole in the eardrum and inserts a tube. The tube helps fluid drain.
Most of the time, children recover quickly and have little pain or other symptoms after the surgery. Your child will probably be able to go back to school or child care the next day.
Adenoid and tonsil removal
Adenoid removal (adenoidectomy) may help some children who have repeat ear infections or fluid behind the eardrum. Children younger than 4 don't usually have their adenoids taken out unless they have severe nasal blockage.
To treat chronic ear infections, experts recommend removing adenoids only after ear tubes and antibiotics have failed. Removing adenoids may improve air and fluid flow in nasal passages. This may reduce the chance of fluid collecting in the middle ear, which can lead to infection.
When used along with other treatments, removing adenoids can help some children who have repeat ear infections.
Learn more
Related Information
- Blocked Eustachian Tubes
- Choosing Child Care
- Colds
- Ear Canal Problems (Swimmer's Ear)
- Ear Problems and Injuries, Age 11 and Younger
- Ear Problems and Injuries, Age 12 and Older
- Hand-Washing
- Labyrinthitis
- Quick Tips: Safely Giving Over-the-Counter Medicines to Children
- Respiratory Syncytial Virus (RSV) Infection
- Using Antibiotics Wisely
Credits
Current as of: October 27, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: October 27, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
This information does not replace the advice of a doctor. Ignite Healthwise, LLC disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use and Privacy Policy. Learn how we develop our content.
To learn more about Ignite Healthwise, LLC, visit webmdignite.com.
© 2024 Ignite Healthwise, LLC.