Our Health Library information does not replace the advice of a doctor. Please be advised that this information is made available to assist our patients to learn more about their health. Our providers may not see and/or treat all topics found herein.
Sleep Apnea
Condition Basics
What is sleep apnea?
Sleep apnea means that breathing stops for short periods during sleep. When you stop breathing or have reduced airflow into your lungs during sleep, you don't sleep well and you can be very tired during the day. The oxygen levels in your blood may go down, and carbon dioxide levels go up. It may lead to other problems, such as high blood pressure and heart disease.
Sleep apnea can range from mild to severe, based on how often breathing stops during sleep. For adults, breathing may stop as few as 5 times an hour (mild apnea) to 30 or more times an hour (severe apnea).
Obstructive sleep apnea is the most common type. This most often occurs because your airways are blocked or partly blocked. Central sleep apnea is less common. It happens when the brain has trouble controlling breathing. Some people have both types. That's called complex sleep apnea.
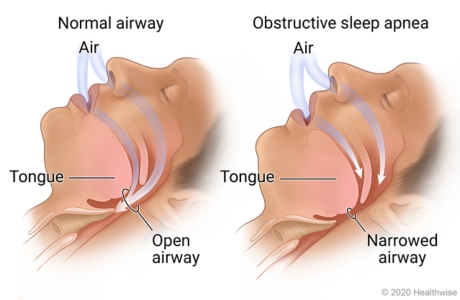
Blocked or narrowed airways in your nose, mouth, or throat can cause sleep apnea. Your airway can become narrowed when your throat muscles and tongue relax during sleep.
What are the symptoms?
The main symptoms of sleep apnea are feeling extremely sleepy during the day, not feeling rested after a night's sleep, or waking up with a headache. If you have a bed partner, they may notice that during sleep you stop breathing, often snore loudly, gasp or choke, or toss and turn.
How is sleep apnea diagnosed?
Your doctor will examine you and ask about your past health. Your doctor may ask you or your bed partner about your snoring and sleep behavior and how tired you feel during the day. Your doctor may suggest a sleep study. You may have other tests to find out what's causing sleep apnea.
How is sleep apnea treated?
Sleep apnea is often treated with a CPAP machine or other machine that prevents your airways from closing during sleep. Oral or nasal breathing devices may also help. A nerve stimulation device may be implanted in the chest to keep the airway open. Surgery to remove tissues blocking the throat may be an option.
Health Tools
Health Tools help you make wise health decisions or take action to improve your health.
Cause
There are two main types of sleep apnea. Obstructive sleep apnea is caused by blocked or narrowed airways in your nose, mouth, or throat. Your airway can become blocked when your throat muscles and tongue relax during sleep. Central sleep apnea is caused by a problem with how the brain signals the breathing muscles.
What Increases Your Risk
Certain things increase your risk for obstructive sleep apnea. These include:
- Obesity.
People who have sleep apnea are more likely to be obese. Obesity is the factor most likely to lead to sleep apnea.
- Neck circumference.
People who are overweight may have extra tissue around their neck, adding to their risk for sleep apnea. The risk increases for a man whose neck measures more than 17 in. around and for a woman whose neck measures more than 16 in. around.
- Family history.
If other members of your family have sleep apnea, you are more likely to have it than someone who doesn't have a family history of it.
- Enlarged tissues of the nose, mouth, or throat.
Enlarged tissues in the nose, mouth, or throat can block your airway while you sleep, making sleep apnea more likely. Surgery can sometimes correct the blockage and improve sleep apnea.
- Aging.
Sleep apnea increases as people get older.
- Being male.
Sleep apnea is more common in men.
- Menopause.
Sleep apnea tends to occur more often in women who have been through menopause than in women who have not. After menopause, women get sleep apnea at a rate similar to men.
- Bone deformities.
Bone deformities of the nose, mouth, or throat can interfere with breathing, causing sleep apnea. Some people who have sleep apnea have a small, receding jaw. Surgery can sometimes correct these deformities and improve sleep apnea.
- Use of alcohol or medicine.
Drinking alcohol or taking certain medicines before going to sleep can increase the risk for sleep apnea. Medicines include some types of sleeping pills, opioids, and sedatives.
- Sleeping on your back.
Sleeping on your back may make sleep apnea worse.
- Smoking.
Smoking can increase your risk for sleep apnea, because the nicotine in tobacco relaxes the muscles that keep the airways open.
- Disorders of the hormone (endocrine) system.
Disorders that may increase your risk include hypothyroidism and acromegaly.
Prevention
You can help prevent obstructive sleep apnea if you try the following ideas.
- Don't use alcohol or certain medicines before bed.
Medicines to avoid include sleeping pills, opioids, and sedatives. These can relax your throat muscles and slow your breathing.
- Have a healthy lifestyle.
Eat sensibly, exercise, and stay at a healthy weight.
- Quit smoking.
The nicotine in tobacco relaxes the muscles that keep the airways open. If you don't smoke, those muscles are less likely to collapse at night and narrow the airways.
Learn more
Symptoms
There are symptoms of sleep apnea that you may notice and symptoms that others may notice when you're asleep.
Symptoms you may notice include:
- Feeling extremely sleepy during the day.
- Feeling unrefreshed or tired after a night's sleep.
- Problems with memory and concentration, or mood changes.
- Morning headaches.
- Getting up often during the night to urinate.
- A dry mouth or sore throat in the morning.
If you have a bed partner, they may notice that you:
- Have episodes of not breathing.
- Snore loudly. Almost all people who have sleep apnea snore. But not all people who snore have sleep apnea.
- Toss and turn during sleep.
- Have nighttime choking or gasping spells.
Symptoms in children
Children who have sleep apnea nearly always snore. But unlike adults with sleep apnea, they may not seem very sleepy during the day.
In younger children, other symptoms include:
- Mouth breathing.
- Sweating.
- Feeling restless.
- Waking up a lot.
In older children, other symptoms may also include:
- Bed wetting.
- Doing poorly in school.
- Behavior problems.
- A short attention span.
- Not growing as quickly as they should for their age. This may be the only symptom in some children.
In rare cases, sleep apnea in children can cause developmental delays and failure of the right side of the heart (cor pulmonale).
Learn more
What Happens
Obstructive sleep apnea causes your airway to narrow or close off, reducing or stopping breathing for short periods during sleep.
If your breathing stops, you may make grunting, gasping, or snorting sounds and restless body movements. As breathing resumes, loud snoring starts. This may happen many times during a night.
The more often it happens, the more severe your sleep apnea is. Sleep apnea is called either mild, moderate, or severe.
Because sleep apnea disturbs your sleep, it can make you very tired during the day. So if you have sleep apnea, you may:
- Be more likely to have a car accident.
- Do poorly at school or work and have trouble concentrating.
- Have memory problems.
- Have personality changes, anxiety, and depression.
- Lose the desire for sex.
Complications of obstructive sleep apnea
When you stop breathing because of obstructive sleep apnea, the oxygen levels in your blood go down and carbon dioxide levels go up. This makes your heart and blood vessels work harder and can affect your heart rate and nervous system. That in turn may:
- Lead to other problems, such as high blood pressure and heart disease.
- Make these other problems worse and harder to treat.
- Raise your risk of having high blood pressure in the lungs (pulmonary hypertension).
- Raise your risk of having a stroke.
- Make it harder for people with diabetes to control blood sugar.
When to Call a Doctor
Call your doctor if:
- You or your bed partner snores loudly and heavily and feels sleepy during the day.
- You notice that your bed partner stops breathing, gasps, or chokes during sleep.
- You sometimes fall asleep at the wrong times, such as while you are talking or eating. Do not drive when you are drowsy.
- Your child snores, has trouble breathing while sleeping, sleeps restlessly, wakes up often, or is very sleepy during the day.
Watchful waiting
Watchful waiting is a wait-and-see approach. If you get better on your own, you won't need treatment. If you get worse, you and your doctor will decide what to do next. Watchful waiting may be right for you if you snore but are not excessively sleepy during the day.
But watchful waiting may not be right if you notice that your sleep partner snores loudly and heavily, is restless during sleep, and is sleepy during the day. If you think your sleep partner may have periods when breathing stops, suggest that they talk with a doctor.
Exams and Tests
Your doctor will probably do a physical exam and ask about your past health. The doctor may also ask you or your bed partner about your snoring and sleep behavior and how tired you feel during the day.
Your doctor may suggest a sleep study. Sleep studies are a series of tests that look at what happens to the body during sleep. They check for how often you stop breathing or have too little air flowing into your lungs during sleep. They also find out how much oxygen you have in your blood during sleep.
A sleep study may take place in your home. Or it might take place at a sleep center, where you will spend the night.
If your sleep apnea doesn't improve with treatment, you may have more tests to find out what's causing it.
Diagnosing sleep apnea in children
To diagnose sleep apnea, the doctor will gather information about your child's symptoms and general health.
- During a routine checkup, your doctor will ask you and your child about snoring. If your child snores, be sure to tell your doctor.
- A complete sleep study usually is needed to find out if your child has sleep apnea and isn't just snoring.
- Children may need to see a specialist if they have sleep apnea.
Learn more
Treatment Overview
Sleep apnea is often treated with machines that deliver air through a mask to help keep your airways open. These include:
- Continuous positive airway pressure (CPAP). This increases air pressure in your throat. It keeps your airway open when you breathe in. It's the most common device.
- Bilevel positive airway pressure (BPAP). You may also hear this called BiPAP. This uses different air pressures when you breathe in and out.
- Adaptive servo ventilation (ASV). It senses pauses in breathing and adjusts air pressure. It's mostly used for central sleep apnea.
You can also try oral breathing devices or nasal devices. Surgery may be an option for some people. Surgery may be done to implant a nerve stimulation device in the chest that helps keep the airway open. Surgery can also be done to remove enlarged tissues that are blocking the throat.
Treating sleep apnea in children
Enlarged tonsils or adenoids are a common cause of sleep apnea in children, so surgery to remove them is usually the first treatment. Children may also be treated with CPAP or corticosteroid medicine. In some cases, a dental device that widens the mouth can help. Children who are overweight are encouraged to lose weight.
Learn more
Self-Care
Lifestyle changes can help treat obstructive sleep apnea. Here are some changes to think about.
- Lose weight.
Weight loss should be part of managing sleep apnea. If you are overweight and have sleep apnea, nutritional counseling, daily activity, and other treatments may help.
- Sleep on your side.
It may help mild apnea.
- Prop up the head of your bed.
- Limit the use of alcohol and medicine.
Drinking alcohol or taking certain medicines, especially sleeping pills, opioids, or sedatives, before sleep may make symptoms worse.
- Get plenty of sleep.
Apnea episodes may be more frequent when you have not had enough sleep.
- Quit smoking.
The nicotine in tobacco relaxes the muscles that keep the airways open. If you don't smoke, those muscles are less likely to collapse at night and narrow the airways.
- Promptly treat breathing problems.
Things like a stuffy nose caused by a cold or allergies can make apnea worse.
- Wear compression stockings if your doctor recommends them.
People who have sleep apnea and tend to have swelling in their lower legs and ankles may be helped by wearing compression stockings during the day. This may prevent a buildup of fluid and swelling of the tissues in the nose and throat at night.
Learn more
CPAP and Other Devices
CPAP
Continuous positive airway pressure (CPAP) is nearly always the first medical treatment for sleep apnea. CPAP is a machine that prevents your airways from closing during sleep.
CPAP can:
- Decrease daytime sleepiness. If you still feel sleepy during the day while using CPAP at night, tell your doctor.
- Lower daytime and nighttime blood pressure.
It may take time for you to be comfortable using CPAP. You may find that you want to take off the mask, or you may find it hard to sleep. If you can't get used to CPAP, talk to your doctor. You might be able to try another type of mask or make other adjustments.
Some CPAP devices automatically adjust air pressure or use different air pressures when you breathe in or out. They are easier and more comfortable for some people to use.
Sometimes medicine that helps you stay awake during the day may be used along with CPAP.
If you use CPAP, or another machine to help you breathe, you need to use it every night and while you nap. If you don't use it, your symptoms will return right away.
Oral and nasal breathing devices
Mouth devices, nose devices, or nerve stimulation devices are sometimes used to treat obstructive sleep apnea.
Oral devices (also called oral appliances) push the jaw or hold the tongue forward. This makes the airway larger and improves airflow. It also reduces the chance that tissue will collapse and narrow the airway when you breathe in. Oral devices may be used for people who have mild to moderate sleep apnea. They may also be used for people with severe sleep apnea who find that continuous positive airway pressure (CPAP) doesn't work for them.
Examples of oral devices include a mandibular repositioning device (MRD) or a tongue-retaining device. A dentist will shape the device to fit your mouth.
Your doctor may suggest that you use nasal devices (such as nose strips or disks) to help keep your airways open while you sleep. Nose strips widen the nostrils and improve airflow. Nasal disks have a valve that makes it harder for you to breathe out. This causes a little back-pressure in the airways that may help keep them open.
You can get many of these oral or nasal devices without a prescription. Talk to your doctor or pharmacist about your options.
A nerve stimulation device may be an option for some people. It is implanted in the upper chest with a surgery. The device senses the breathing pattern and mildly stimulates the airway muscles to keep the airway open.
Learn more
Related Information
Credits
Current as of: July 31, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: July 31, 2024
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
This information does not replace the advice of a doctor. Ignite Healthwise, LLC disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use and Privacy Policy. Learn how we develop our content.
To learn more about Ignite Healthwise, LLC, visit webmdignite.com.
© 2024 Ignite Healthwise, LLC.